Douglas F. Milam M.D.
Urologic Surgery
- Home
- About Us
- Surgical Procedures

- Evaluation of Voiding Dysfunction

- Patient Information

- IPSS-AUA Symptom Score
- Sexual Function Questionnaire
- Deactivate a Urinary Sphincter
- VPEC
- Overnight Surgical Stay
- Post-operative Instructions Urethral Stricture Repair
- Post-operative Instructions Penile Implant
- Post-operative Instructions Artificial Urinary Sphincter
- Post-operative Instructions Placement of Male Sling
- Post-operative Instructions Penile Curvature Repair
- Post-procedure Instructions Vasectomy
- Mechanism of Erection
- Statement on Urologic Pain
- Schedule a Consultation
- Directions

- Urologic Images
- Web References
Male Continence Procedures
Surgical Procedures to Improve Continence in Men
Evaluation of incontinence begins with a history of the symptoms and usually includes urodynamic testing and cystoscopy. Our goal is to evaluate the cause and extent of your condition, and to discuss the surgical therapies that are most likely to improve your condition. We do discuss nonsurgical treatment, but the overwhelming majority of our patients have tried and failed any available medicines (pills) before coming to our practice. Once we know the specifics of your condition we can recommend treatments that have the highest likelyhood of success. These include surgical implantation of a urethral sling or artificial urinary sphincter, implantation of an Interstim Continence Control device, or placement of urethral bulking agents.
Overview
Incontinence in men is more common than most people realize. Often it presents with the loss of a few drops of urine. While bothersome, that degree of incontinence does not meet most people's threshold for requiring surgical intervention. In our practice we typically see patients with much more severe urinary incontinence who are looking for a surgical option to improve their condition.
Many of our patients experience loss of urinary control due to either surgical procedures or radiation therapy given to treat cancer. There are many reasons why patients develop incontinence following cancer treatment. Even with optimal treatment for their cancers, patients can still develop side-effects such as incontinence. The length of time that one should wait following cancer treatment before pursuing treatment for incontinence depends on the degree of incontinence, the type of treatment that was given, and the physical situation of the individual patient. We are happy to advise individual patients about best time to pursue work-up and possible treatment.
Incontinence may also be due to conditions that patients develop. These include non-cancerous growth of the prostate (BPH), neurologic processes such as Parkinson's disease, multiple sclerosis, spinal cord injury, and spinal disc disease.
Incontinence Evaluation
Evaluation of incontinence begins with a history of the symptoms and usually includes urodynamic testing and cystoscopy. Our goal is to evaluate the cause and extent of your condition, and to discuss the surgical therapies that are most likely to improve your condition. We do discuss nonsurgical treatment, but the overwhelming majority of our patients have tried and failed any available medicines (pills) before coming to our practice. Once we know the specifics of your condition we can recommend treatments that have the highest likelyhood of success. These include surgical implantation of a urethral sling or artificial urinary sphincter, implantation of an Interstim Continence Control device, or placement of urethral bulking agents
Artificial Urinary Sphincter (AUS)
Patients with more severe incontinence usually require an artificial urinary sphincter (AUS). We have extensive experience placing the artificial urinary sphincter for first time implant patients, in the setting where revision of an existing implant is required, and also for patients who have had an artificial sphincter in the past but lost the device for any reason.
The AUS device usually produces the most improvement in continence. Patients soaking 2 pads per day to as much as 14 pads per day usually have substantial improvement in their continence. The second photo below illustrates the entire AUS device. The compressive urethral cuff is deflated by squeezing the pump located in the scrotum. The device is tested in the operating room, then deactivated for six weeks during recovery. After six weeks the device is activated in the office and the patient learns how to use his device. Once activated, the urethral cuff compresses the urethra working to improve patient continence. When the patient feels that his bladder is full he squeezes the pump through the scrotal wall. This opens the urethra by pumping the salt water fluid from the cuff into the pressure regulating balloon. The patient then urinates and the cuff automatically refills over a 60 to 90 second period. The antibiotic coated (gives the yellow color) cuff is shown in the third photo below. Placement of the artificial urinary sphincter (AUS)involves an overnight hospital stay. Post-operative instructions for the artificial urinary sphincter (AUS) can be reviewed by clicking here. Detailed drawings and operative photographs shown below help to explain the procedure.
Male Sling Procedure
A urethral sling is a small rectangular synthetic mesh that is placed under the urethra. The procedure is useful for patients with mild/moderate incontinence and is done as a day surgical procedure. Urodynamic testing is often very helpful in identifying whether a patient is an appropriate candidate for a sling procedure. The drawing and photos below show the position of a sling supporting the urethra. Please click here to review post-operative instructions for the male sling procedure.
Interstim Implantation and Botox Injection
Interstim and Botox injection are treatments to control incontinence and bladder urgency/frequency caused by bladder contraction when the bladder should be quiet. This condition is termed bladder overactivity, or involuntary bladder contraction and is very different than urinary sphincter dysfunction described above. The bladder can squeeze forcefully leading to incontinence even in men with competent urethral sphincter function. Urodynamic testing can help differentiate whether the problem is with the urinary sphincter or bladder overactivity. If the problem is overactivity, but the sphincter function appears adequate, there are both medications and surgical procedures to help decrease the frequency and force of bladder overactivity. Many men coming into our practice have already tried and failed a range of medications for overactive bladder. If you have not tried these medications we likely would try one or more of them over a 1 to 3 month interval. If you have used the medications in the past without success, then it is time to consider surgical treatment. That would be either Interstim implantation or Botox injection into the bladder wall.
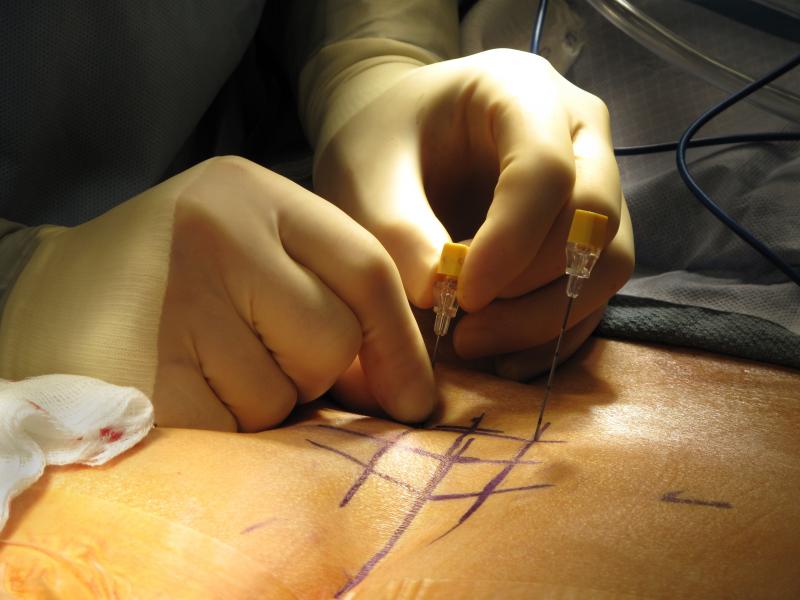
Interstim uses a technique called neuromodulation. We use a special wire to stimulate the nerves going to and from the bladder with a special electrical current (neuromodulation). Interstim is a two step procedure. First we place the wire in to the vicinity of the nerves. We then evaluate your response over the next week. If you have a good response then we usually proceed with implantation of an Interstim device. There are two different ways to do the first stage of the procedure. Both have relative advantages and disadvantages. If you are a candidate for Interstim therapy, we will discuss these options in detail. The bottom photo shows the needle being inserted into the vicinity of the nerve. We often test both the right and left sides to determine the optimum site for placement of the wire.
ARTIFICIAL URINARY SPHINCTER (AUS)
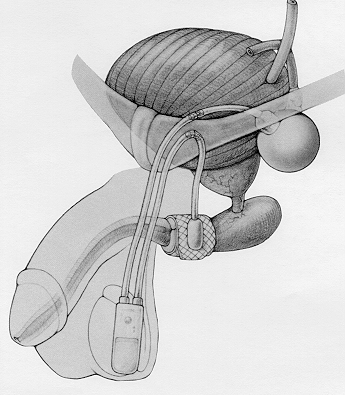
Artificial urinary sphincter (AUS) diagram. All parts of the device are implanted inside the body. The pressure regulating balloon, urethral cuff, and pump are shown here connected by tubing.

This photograph shows the three parts of the AUS. Shown from left to right are the urethral cuff, an empty pressure regulating balloon, and the pump. Different sizes of urethral cuffs are used depending on the measured circumference of the patients urethra. The pressure regulating balloon is filled with about 23ml of saline (salt water) during the operation. The pressure regulating balloon generates a carefully selected amount of pressure causing the urethral cuff to gently squeeze the urethra. That is how an AUS improves continence. The pump which is placed in a dependent portion of the scrotum is shown on the right. Compression of the bottom half of the pump causes fluid to be withdrawn from the urethral cuff, opening the urethra and allowing the patient to urinate. The urethral cuff and the pump are antibiotic coated (yellow color) to minimize the risk of infection. The pressure regulating balloon cannot be antibiotic coated at this time due to manufacturing considerations.




Once the plane has been developed between the urethra and the underlying corporal body, we measure the circumference of the urethra in order to select the proper size urethral cuff. In this case, the urethra measures almost 4 3/4 centimeters. A 5cm cuff would be used in this case. This urethra is more normal than many we see. Prior surgery or radiation therapy often leads to loss of urethral tissue (atrophy). In severe cases of atrophy we often place the urethral cuff behind the next layer backing the urethra (transcorporal placement) instead of the standard placement shown immediately below.

The artificial urinary sphincter cuff is shown here surrounding the urethra. This is a typical placement where the urethra is circumferentially separated from surrounding tissue for about 1.5 centimeters. The cuff is passed around the urethra and the snap connection is made at the tubing take-off. The next step of the operation is to rotate the tubing take-off to the left (patients right) and to bring the tubing to the upper incision where all tubing connections are made.

Transcorporal AUS Cuff Placement: This extreme close-up photograph shows the urethra running top to bottom in the center of the photo. The patient has very severe atrophy (loss of tissue) of the urethra due to prior surgery and radiation therapy. In selected cases like this we may choose to perform a transcorporal cuff placement. This provides an additional tissue layer behind the urethra in an effort to minimize the chance of erosion of the cuff into the compromised urethral tissue. The two purple marks lateral to the urethra on the corporal bodies indicate the site of the incisions. We will open the corpora in order to create a tunnel under the urethra within the corporal body.

The right angle clamp has been passed within the corporal body, but immediately behind the urethra. This provides an extra layer of tissue to minimize the risk of urethral cuff erosion in patients who have experienced substantial urethral atrophy. The clamp grasps a flange on the cuff made for this purpose and passes the cuff around the back side of the urethra. The snap mechanism shown two photographs above completes the urethral cuff placement.

Here is a view looking through a cystourethroscope into the urethra of a patient with an AUS. The cuff of the AUS completely encircles the urethra and is only a few millimeters under the urethral lining. In this case the cuff is 50% closed. The urethral channel can be seen as the dark area on the other side of the cuff. It is very important to fully empty the urethral cuff before attempting to pass a catheter into the bladder.

This is a view of the outline of the AUS pump through the scrotal wall 4.5 months after the device was implanted. The AUS urethral cuff remains closed until the pump bulb is compressed. Pressing the pump bulb forces the fluid (saline, salt water) in the cuff through the pump and into the pressure regulating balloon. With the cuff decompressed, the patient can urinate normally. The urethral cuff refills under pressure in 60-90 seconds restoring continence.
The AUS can be deactivated (turned off) by fully compressing the pump bulb 2-3 times and then quickly and firmly compressing the deactivation button. The pump bulb should remain at least 1/2 empty. If each side of the pump bulb has an indentation (dimple) after 2 minutes the device can safely be considered deactivated. Click here for detailed instructions of how to deactivate the AUS.
MALE SLING
A male sling is a synthetic hammock surgically implanted to support the urethra.

This overview slide shows the sling passing through the holes in the pelvic bone (Obturator Foramen) and passing under and supporting the bulbar urethra. A sling does not add sphincter function to the urethra, but hopefully allows the patients own sphincter muscle to function more effectively.

The male sling is implanted through a small incision in the perineum under the scrotum. We incise the overlying tissue layers until the urethra is encountered (center of the photo). Fibers from the perineal body attach to the urethra. The most distal (downstream on the urethra) of these fibers have been removed and a purple mark was placed in that location. This is the location where the sling will be implanted.

Synthetic Mesh of a bone anchored male sling implanted in the perineum. Several layers of tissue are closed over the sling in addition to the skin layer.
INTERSTIM
Treatment for urinary frequency, urgency, and urinary retention
Interstim is a technique where a low amplitude electrical current is used to neuromodulate the nerve signals coming from and going to the bladder. It is performed as a two stage procedure.
On each side of the back of the pelvis there are 4 holes in the bone, or foramina. Here we see needles inserted into the third foramen on both right and left sides. A special wire is passed through the needles into the region of the nerves. Once testing is complete, we remove the needles leaving one or both wires in place. The wire is connected to a special cell phone sized generator box that the patient wears for a one week trial. Interstim is useful for urinary urge incontinence, urinary urgency and frequency, and urinary retention.

If the one week Interstim test period is successful, a permanent generator can be implanted in the operating room. This photo shows an Interstim II device being implanted. This generator is connected to the lead that stimulates the nerves coming to and from the bladder and has a battery life of about 3 years.
Copyright 2010-2015 Milam Urology. All rights reserved.