Douglas F. Milam M.D.
Urologic Surgery
- Home
- About Us
- Surgical Procedures

- Evaluation of Voiding Dysfunction

- Patient Information

- IPSS-AUA Symptom Score
- Sexual Function Questionnaire
- Deactivate a Urinary Sphincter
- VPEC
- Overnight Surgical Stay
- Post-operative Instructions Urethral Stricture Repair
- Post-operative Instructions Penile Implant
- Post-operative Instructions Artificial Urinary Sphincter
- Post-operative Instructions Placement of Male Sling
- Post-operative Instructions Penile Curvature Repair
- Post-procedure Instructions Vasectomy
- Mechanism of Erection
- Statement on Urologic Pain
- Schedule a Consultation
- Directions

- Urologic Images
- Web References
Deactivate a Urinary Sphincter
The artificial urinary sphincter (AUS) can produce life changing improvement in the quality of life of men with severe incontinence due to intrinsic sphincter dysfunction. Unfortunately, the AUS may be damaged by the passage or presence of a urethral (Foley) catheter. The AUS must be fully deactivated before placement of a urethral catheter and one should assure that the AUS remains deactivated for the entire time that the urethral catheter remains in place. Placement of a urethral catheter without deactivation of the device causes compression of urethral tissue between the catheter and the compressive cuff decreasing blood flow to the urethra. With loss of urethral tissue, the cuff may erode into the urethral lumen necessitating removal of the device. The bottom line, assuring that a dimple is present in the AUS pump bulb before catheter passage and that a dimple remains present while the catheter is indwelling will protect urethral tissue as much as possible. Information below illustrates how to deactivate the AUS.
Deactivation and later activation of the AUS is performed by manipulating the scrotal pump. This is a two handed operation. Fingers from one hand should grasp the tubing just above the pump to stabilize the device while the thumb and forefinger of the other hand compress the pump three times. This pumps all of the fluid from the cuff into the pressure regulating balloon. One then quickly and vigorously compresses the deactivation button preventing return of fluid into the cuff. Deactivation can be confirmed by examining the pump 90 seconds later. The dimple will remain in the pump bulb if the device is deactivated. If the pump bulb refills, the device is not deactivated.
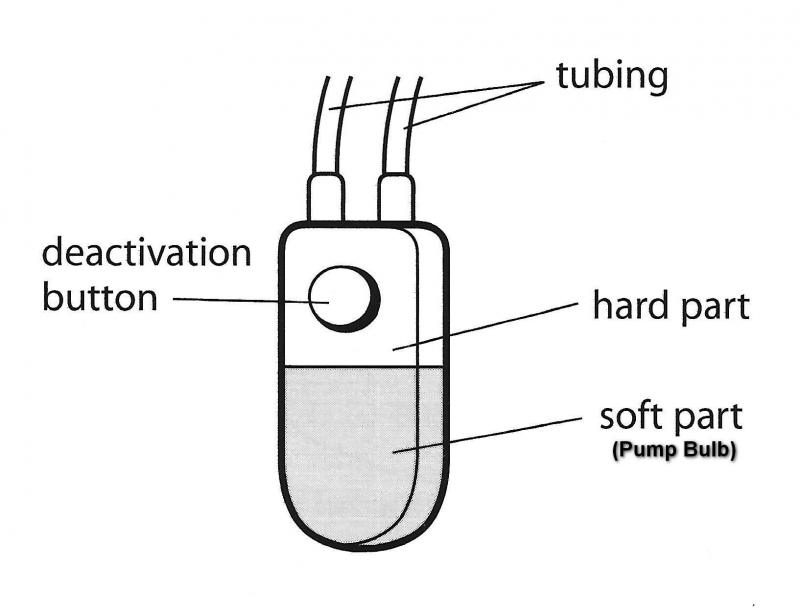
The AUS pump has an upper hard part that contains the deactivation button and a lower soft part where the pump bulb is compressed to pump fluid out of the urethral cuff.
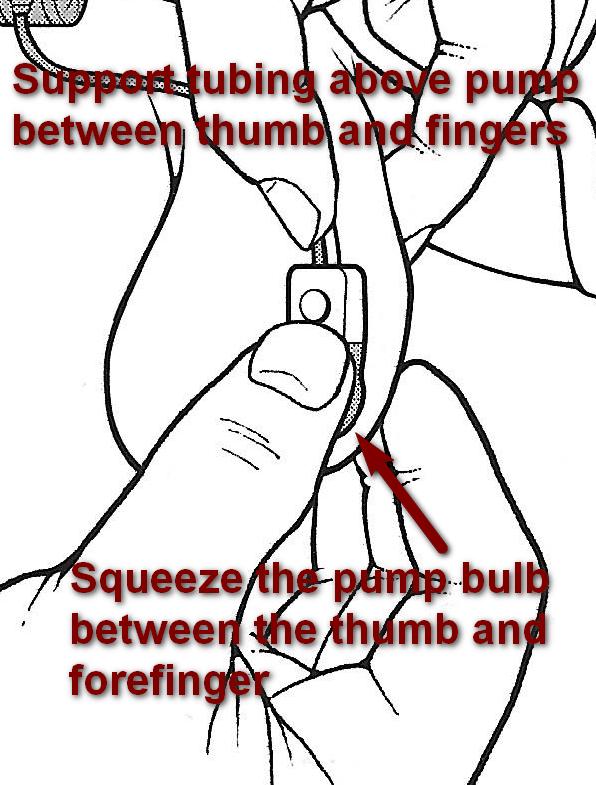
It is important to support the pump by holding the tubing as it exits the upper part of the pump. The other hand is free to compress the pump bulb. We recommend compressing the pump bulb three times. The first pump will be a full compression, the secomd pump will be about 2/3 of a compression and very little fluid will be moved by the third pump.

After the third pump, the soft pump bulb will have a large dimple. At that point the deactivation button should be very firmly compressed for 1/3 of a second. One can feel the button moving, however, it quickly returns to the original location.

Compression of the deactivation button is firm and quick. One should then wait 90 seconds to make sure that the dimple remains in the pump bulb. If the dimple remains, the device is deactivated. If not, the device is active and the deactivation procedure should be repeated.
Copyright 2010-2015 Milam Urology. All rights reserved.